


Received: 30-Nov-2022, Manuscript No. GJDOH-22-82937; Editor assigned: 02-Dec-2022, Pre QC No. GJDOH-22-82937 (PQ); Reviewed: 16-Dec-2022, QC No. GJDOH-22-82937; Revised: 23-Dec-2022, Manuscript No. GJDOH-22-82937 (R); Published: 30-Dec-2022, DOI: 10.15651/2449-1918.22.9.012
The collective genome of the bacteria that live in the mouth cavity is known as the oral microbiome. It is the second biggest microbial colony in humans, behind the gut. They have an incredible range of anticipated protein activities when compared to other body locations. A core microbiome and a variable microbiome make up the human microbiome. All people share the same core microbiome, yet each person has a different variable microbiome based on their lifestyle and physiological makeup. Because the mouth cavity is constantly in contact with the outside world, the oral microbiome is varied in its makeup. Temperatures, nutrition, pH, feeding patterns are major elements that help in the creation of oral microbiota. In order to analyse the oral microbiota, both culture-dependent and culture-independent techniques have been used. Gene-based approaches have been used to expand understanding about the oral microbiome, including PCR amplification methods, random amplicon cloning, PCR-RELP (Polymerase Chain Reaction- Restriction Fragment Length Polymorphism), T-RELP (Terminal Restriction Fragment Length Polymorphism), DGGE (Denaturing Gradient Gel Electrophoresis), and DNA microarray analysis (Deoxyribonucleic Acid).
Some indigenous microflora populations are vanishing as a result of ongoing advancements in pharmacological research and medical technology. The microbial communities found in the mouth and in faeces are said to be the most diverse forms. Changes in micro-ecology have a direct impact on a person's microbiota since exposure to various factors, such as antibiotics, immunisations, active or passive smoking, etc., differs from person to person and hence has different effects. One sign of a diminishing microbiota is the disappearance of Helicobacter pylori in humans due to changes in the reasons outlined above. The phage type in the mouth is constant during the whole life cycle. When certain illnesses are present in the body, new viruses might potentially appear in the mouth. The mumps virus and HIV are the most prevalent. The majority of the oral microbiota is made up of oral bacteria. Streptococcus mutans, Porphyromonas gingivalis, Staphylococcus, and Lactobacillus are typical oral bacteria. The primary element of the oral microbiota and one of the primary elements of dental plaque is mutants. Additionally, it is the primary cause of caries, the most common dental illness with a bacterial cause that affects the hard tissues of the teeth. P. gingivalis is a periodontal pathogen that is a nonglycolytic Gram-negative anaerobic bacterium. If P. gingivalis is left untreated, gums may separate from teeth. A bacteria known as Lactobacillus is capable of fermenting sugar to create lactic acid. It is a collection of microorganisms that reside in the body and enhance the host's health. Yogurt has lactobacilli in it. Sugar is fermented by Lactobacillus, which also generates a significant amount of lactic acid, which is readily cariogenic.
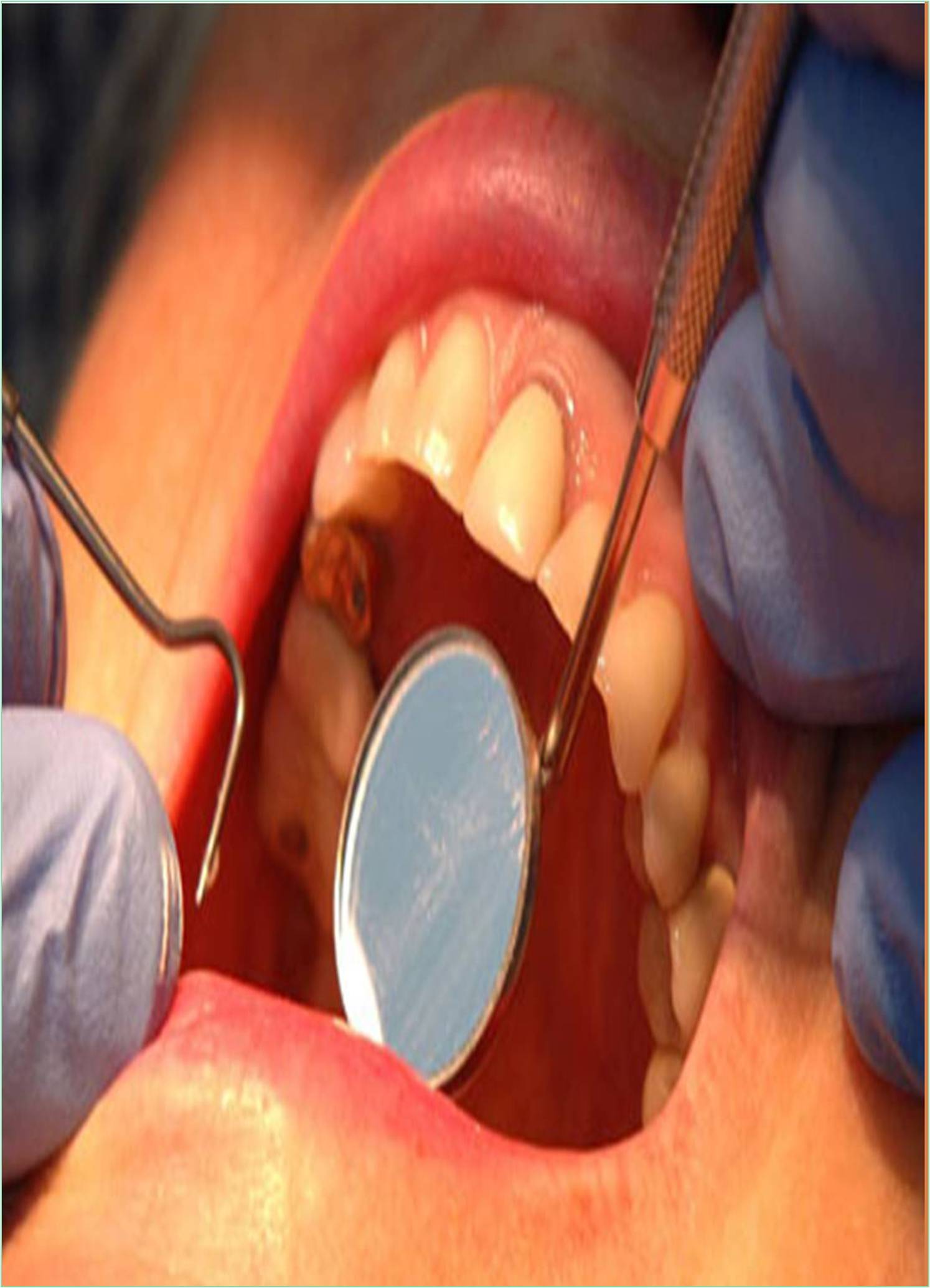
The mouth contains a variety of unique habitats for microbial colonisation, including teeth, the gingival sulcus, connected gingiva, the tongue, cheek, lip, and the hard and soft palate. These oral environments promote the development of very diverse microbial populations and make up a highly heterogeneous biological system. Numerous bacteria may thrive in the warm, moist environment of the mouth, which also provides nutrients obtained from the host, such as saliva proteins, glycoproteins, and Gingival Crevicular Fluid (GCF). The teeth offer exceptional potential for widespread biofilm development and a safe refuge for microbial persistence since they are the only naturally non-shedding surfaces in the human body. Additional non-shedding surfaces in the mouth, such as dental restorations, crown and bridgework, detachable prostheses, and implants, might affect the composition and production of biofilms.
The loss of the oral microbiota can be harmful to a person's health since it supports both oral and overall health. An illustration of this is the action of oral bacteria that produce nitrate-reductase, which has been demonstrated to catalyze the conversion of dietary nitrates to nitrite. After being swallowed, salivary nitrite is further converted to nitric oxide; a potent vasodilator with antimicrobial activity which plays a critical role in sustaining cardiovascular health. Nitrite also promotes the development of stomach mucous. A recent study indicated that prolonged use of dietary nitrates improves vascular function in people with hypercholesterolemia. Nitrate consumption has been reported to lower blood pressure, limit platelet activity, and minimize endothelial dysfunction. These benefits were linked to alterations in the oral microbiota that favored nitrite-reduction-capable organisms. Although dietary nitrates can increase nitrite production, it is also true that nitric oxide in tissues can interact with superoxide radicals produced by immune cells to make peroxynitrite anions, which have been linked to harmful effects on cells such as DNA damage.