


Received: 18-Jul-2022, Manuscript No. GJCMB-22-72499; Editor assigned: 21-Jul-2022, Pre QC No. GJCMB-22-72499 (PQ); Reviewed: 04-Aug-2022, QC No. GJCMB-22-72499; Revised: 11-Aug-2022, Manuscript No. GJCMB-22-72499 (R); Published: 18-Aug-2022, DOI: 10.15651/gjcmb.22.10.010
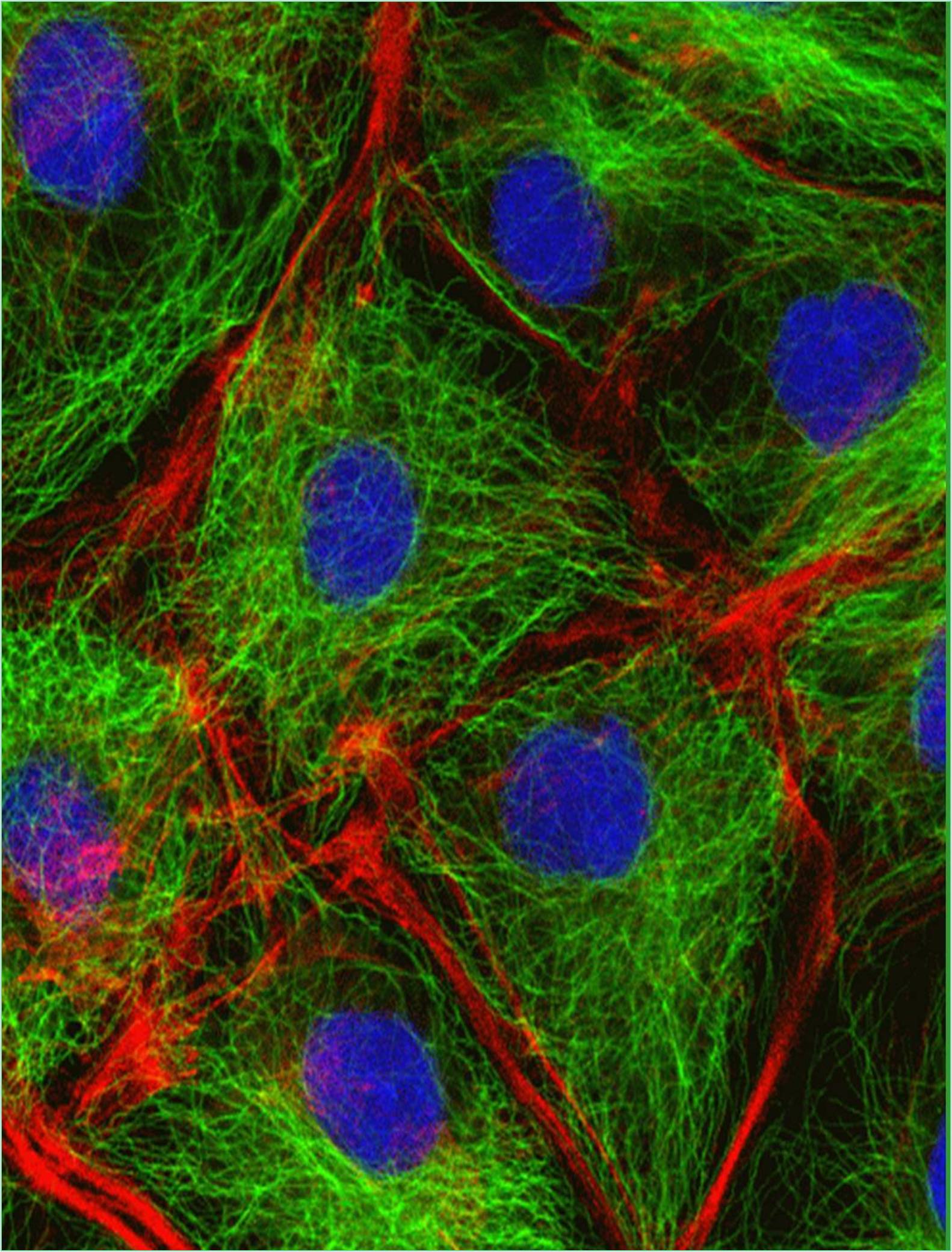
The tissues develop from mesoderm into embryonic ectoderm and endoderm, between the ectoderm and the endoderm is a layer of cells that develops and diversifies to serve a variety of supportive roles. It generates the connective tissues, blood cells and blood arteries of the body in addition to the muscle, kidney and several other organs and cell types. Nearly all tissues rely on blood flow and blood flow depends on endothelial cells, which create the blood vessel linings. Endothelial cells are remarkably capable of changing their composition and quantity to meet local needs. By migrating cells into practically every part of the body, they build a flexible life support system. Tissue growth and healing would not be feasible without the extension and modification of the blood artery network by endothelial cells.
The main blood vessels are arteries and veins, which include numerous layers of smooth muscle cells and a thick, durable wall made of connective tissue (Schrankel et al., 2021). The endothelium an incredibly thin strip of endothelial cells that lines the wall is situated between the wall's outer layers and the basal lamina. Depending on the vessel's diameter and function the amount of connective tissue and smooth muscle in the vessel wall varies but the endothelium lining is always present. Only endothelial cells a basal lamina and a few scatted but strategically placed pericytes make up the walls of the vascular tree's finest branches the capillaries and sinusoids. These are connective tissue cells that wrap around the tiny vessels they are connected to vascular smooth muscle cells.
Endothelial cells therefore line the whole circulatory system from the heart to the smallest capillary and regulate material transit and white blood cell transit into and out of the bloodstream (Sozen et al., 2021). The signals that the endothelial cells send to the surrounding connective tissue and smooth muscle after a vessel has developed continue to be essential in controlling the vessel's form and function. For instance, the endothelial cells can sense the shear stress caused by blood flowing over their surface. By communicating this information to the cells around them, they enable the blood vessel to change its diameter and wall thickness to accommodate the blood flow. By releasing the gas NO to cause the smooth muscle in the vessel wall to relax, endothelial cells also facilitate quick responses to brain impulses for blood vessel dilatation.
Factors Released by the Surrounding Tissues Control Angiogenesis
Nearly every cell in every tissue of a vertebrate is found 50 m to 100 m or less from a capillary. For instance, a wound causes a sudden increase in capillary growth in the area of the injury to meet the high metabolic demands of the healing process. New capillaries proliferate as a result of local irritations and infections, but most of them regress and dissolve after the inflammation goes away.
When endothelial cells enter a tissue, the tissue sends signals to the endothelial cells. The signals are intricate, but a protein called Vascular Endothelial Growth Factor (VEGF) a distant relative of Platelet-Derived Growth Factor plays a significant role (PDGF). Through adjustments to the stability of its mRNA and transcriptional rate, VEGF production can be controlled to tailor blood vessel formation to the needs of the tissue (Zhang et al., 2022). Almost all cell types experience an increase in the intracellular concentration of the active form of a gene regulatory protein called Hypoxia- Inducible Factor (HIF-1), when there is a lack of oxygen. The VEGF gene's transcription is promoted by HIF. The tissue-diffusing VEGF protein is released, where it diffuses and interacts with neighboring endothelial cells.
The oxygen concentration increases, HIF-1 activity decreases, VEGF production is stopped and angiogenesis stops as new blood vessels begin to grow and bring blood to the area (Zhang et al., 2022). As with all signaling systems, it is crucial to turn the signal off properly just as it is to turn it on. The constant breakdown of the HIF-1 protein keeps the concentration of HIF-1 low in healthy, well-oxygenated tissue. This degradation is dependent on HIF-1's ability to be ubiquitylated, which depends on the output of a different gene that is damaged in a condition known as Von Hippel-Lindau (VHL) syndrome. Only one functioning copy of the VHL gene is present at birth in individuals with this disorder (Zhu et al., 2022). As a result, cells with both faulty gene copies develop randomly throughout the body. No matter how much oxygen is present, these cells have high levels of HIF-1, which causes VEGF to continually overproduce. Hemangioblastomas, tumours with thick masses of blood vessels, form as a result.
Schrankel CS, Hamdoun A (2021). Early patterning of ABCB, ABCC, and ABCG transporters establishes unique territories of small molecule transport in embryonic mesoderm and endoderm. Dev Biol. 472:115-124. [Crossref] [Google Scholar] [PubMed]
Sozen B, Demir N, Zernicka-Goetz M (2021). BMP signaling is required for extra-embryonic ectoderm development during pre-to-post-implantation transition of the mouse embryo. Dev Biol. 470:84-94. [Crossref] [Google Scholar] [PubMed]
Zhang G, Ci H, Ma C, Li Z, Jiang W, Chen L, Wang Z, Zhou M, Sun J (2022). Additive Manufactured Macroporous Chambers Facilitate Large Volume Soft Tissue Regeneration from Adipose-derived Extracellular Matrix. Acta Biomater. [Crossref] [Google Scholar] [PubMed]
Zhang X, Liu L, Liu D, Li Y, He J (2022), Shen L. 17β-Estradiol promotes angiogenesis of bone marrow mesenchymal stem cells by upregulating the PI3K-Akt signaling pathway. Comput Struct. Biotechnol J. 20:3864-3873. [Crossref] [Google Scholar] [PubMed]
Zhu S, Zidan A, Pang K, Musayeva A, Kang Q, Yin J (2022). Promotion of corneal angiogenesis by sensory neuron-derived calcitonin gene-related peptide. Exp Eye Res. 109125. [Crossref] [Google Scholar] [PubMed]