


Received: 05-Aug-2022, Manuscript No. GJDOH-22-72145; Editor assigned: 08-Aug-2022, Pre QC No. GJDOH-22-72145 (PQ); Reviewed: 22-Aug-2022, QC No. GJDOH-22-72145; Revised: 29-Aug-2022, Manuscript No. GJDOH-22-72145 (R); Published: 05-Sep-2022, DOI: 10.15651/2449-1918.22.9.006
The human body's teeth are highly mineralized organs. Following tooth eruption, the tooth's hard tissue is repaired or replaced naturally by mineral crystals made of calcium, phosphorus, fluorine, and other inorganic ions. Teeth go through a lifetime process of demineralization and remineralization that, given physiological circumstances, finds equilibrium. The minerals in the teeth are lost when demineralization has place before remineralization, which is the initial stage of caries. Therefore, a viable strategy for preventing and treating caries is speeding up the remineralization process. The development of resin-based dental materials and a better knowledge of how caries and remineralization occur have accelerated the transition from G.V. Black's "preventive extension" idea to a "minimally intrusive" strategy for managing caries. Caries can produce pulpitis, which in turn can result in pulp infection and necrosis. In deep caries care, it is conventional to completely remove carious dentin. Caries-affected dentin is preserved when the caries-infected dentin is removed in minimally invasive dentistry. Remineralizing fillers in resin-based dental materials, such as adhesives and composite resins, may encourage the remineralization of leftover CAD (Computer-Aided-Design) to stop the development of pulp exposure and preserve live pulp.
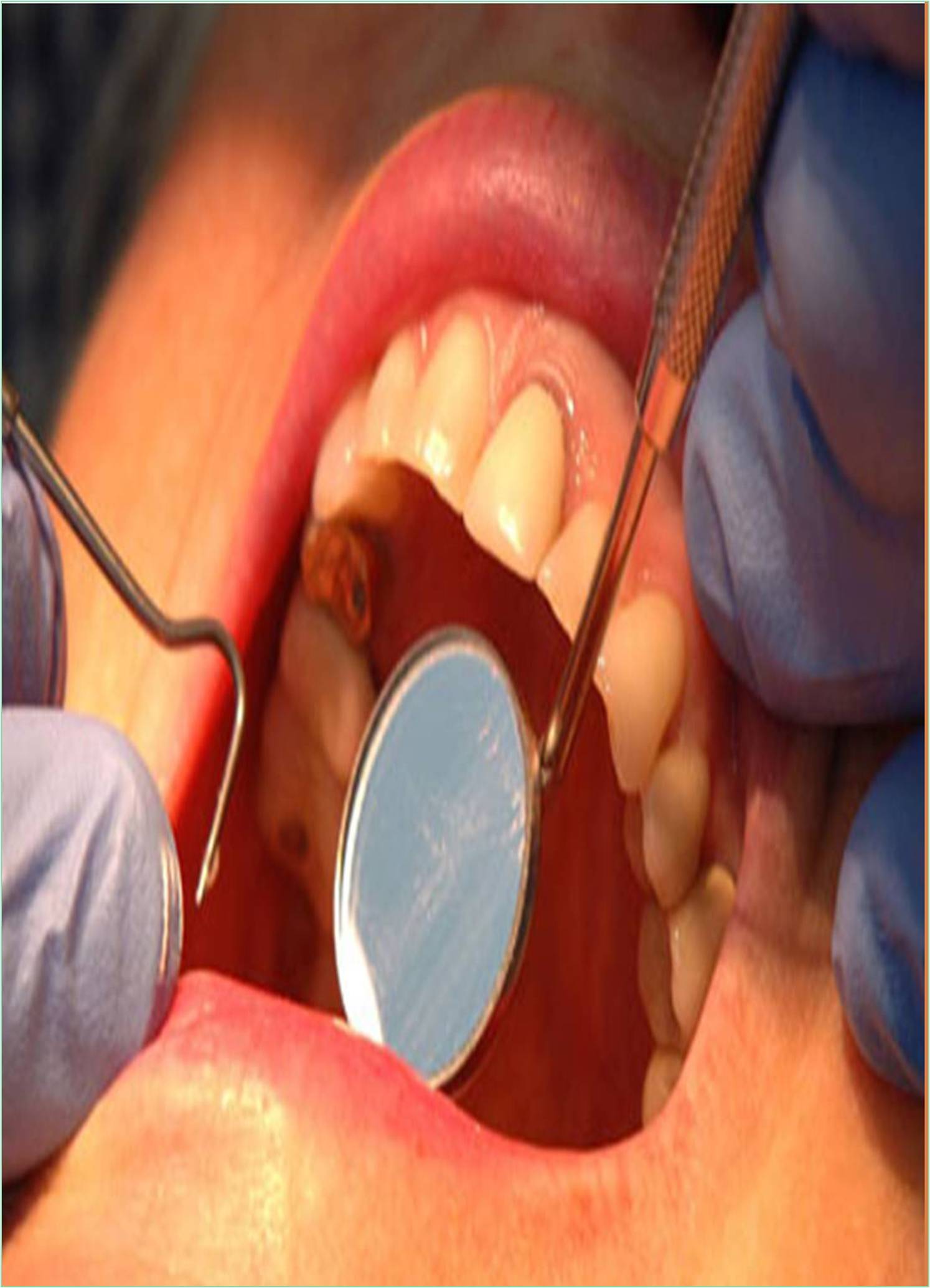
The long-term clinical performance of composite resin restorations is significantly influenced by the quality and durability of adhesive surfaces in enamel and/or dentin. The gold standard for bonding systems is still thought to be the three-step etch-and-rinse adhesive systems due to their shown success in both laboratory and clinical testing. Recent years have seen a simplification in bonding, with solutions combining the primer and bonding agent, the conditioner and primer, or even all three components. The formulation of all modern adhesive systems includes a variety of distinct molecules that serve the same purposes and, as a result, have a similar fundamental bonding mechanism. This mechanism works by replacing the inorganic tooth material with resin monomers that, after setting in place, interlock micromechanically in the tiny pores the substrate has generated. Providing a bond that is equally successful for a variety of dental substrates of diverse natures, such as enamel, sound, caries-affected, or sclerotic dentin, is the major difficulty facing modern dental adhesives. From a clinical standpoint, selective etching of enamel, followed by the application of a mild 10-MDP-based two-step selfetch adhesive to both etched enamel and non-etched dentin, would be the best option for an efficient and more long-lasting bond to the dental substrate when bonding to both enamel and dentin.
As early as 50 years ago, dental remineralization for carious tissue started to receive attention. Remineralizing agents may be used in resin-based materials to extend the lifespan of Resin-Based Composites (RBCs), remineralize CAD, or stop the progression of caries lesions. However, it is not simple to manufacture resinbased materials with remineralizing agents. The early remineralization strategy involved surrounding the caries lesions with a lot of fluoride, calcium, and phosphorus substrates in order to encourage remineralization. Later, to encourage remineralization of the bonding surface, fluoride-releasing composite resins and adhesives incorporating bioactive glass (BG) were utilised. Some academics have advocated the idea of "biomimetic mineralization" to better mimic the structure of real teeth. Bonding interface and CAD remineralization are the current areas of study for biomimetic remineralization techniques in in vitro investigations. The technological challenge in clinical application is how to retain the mechanical qualities while the beneficial components needed for remineralization are progressively released, as well as how to continually supply them. In order to transition the biomimetic remineralization technique from in vitro testing to clinical use, researchers have recommended employing rechargeable nanoparticles for continual ion release and some transportation mechanism, such as mesoporous nanomaterials. Since glass-ionomer cement is water-based and dentine is a tissue that contains water and frequently has a layer of odontoblast tubular fluid on the cut surface, the two materials are compatible. Comparatively incompatible with dentine is resin composite, a hydrophobic substance. An acid-base interaction between a polyalkenoic acid and a fluroaluminosilicate glass caused the initial Glass-Ionomer Cements (GICs) to set. These materials were fragile, thus efforts were undertaken to improve their physical characteristics by adding metal particles, fusing ceramic and metal to produce "cermet," or adding amalgam alloy particles.